Streamlined Pre & Retro Authorization Services for Faster Approvals
Our expert team handles prior and retro authorization requests with accuracy and speed. From paperwork submission to denial resolution, we simplify the process so you can focus on patient care while we ensure timely approvals and secure reimbursements.

What is Prior authorization?

Comprehensive Prior Authorization Services for Faster Approvals
We carefully evaluate the medical necessity and insurance requirements to ensure your authorization request meets all payer guidelines from the start.
Our team manages the complete paperwork process, preparing and submitting accurate documentation to insurance companies without delays.
We actively track and follow up with payers to prevent unnecessary waiting times, ensuring your requests move forward smoothly.
f an authorization is rejected, we promptly notify providers and work on resubmission or appeals to secure approval quickly.
How does Prior Authorization work?
Getting prior authorizations approved involves many people – primarily patients, healthcare professionals, and the patient’s health insurance companies.
Prescription Prior Authorization

Provider Opinion on Prior Authorization
Why is Retro Authorization Important?

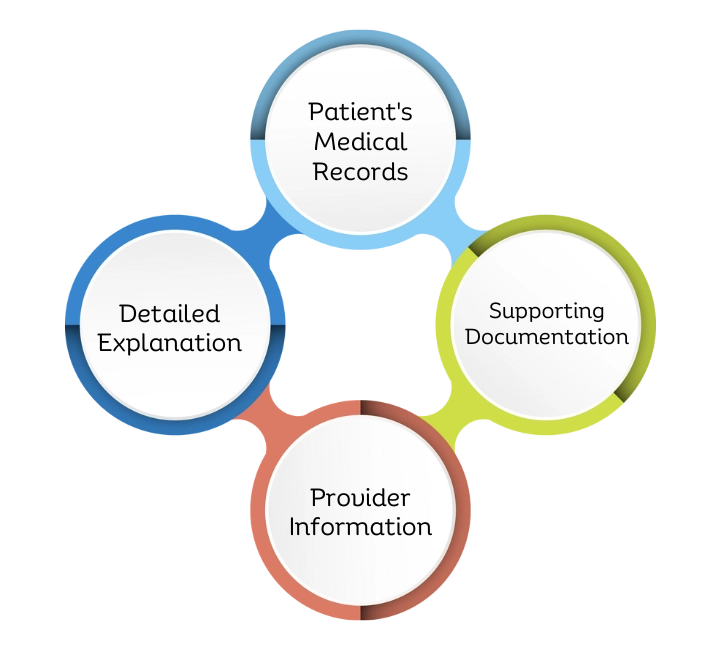
Key Components of a Retro Authorization Request
A retro authorization request requires accurate medical records, proof of medical necessity, and timely submission details. These components ensure faster approvals and reduce the chances of claim denials.
Patient’s Medical Records
Comprehensive documentation of the patient’s medical history and the specific services provided.
Detailed Explanation
A thorough explanation outlining the necessity for retro authorization and why the services were not pre-authorized.
Supporting Documentation
Any additional documentation supporting the retro authorization request, such as test results or physician notes.
Provider Information
Relevant details about the healthcare provider submitting the request, ensuring clarity in the authorization process.
Our Expert Prior Authorization Solutions for Providers

Delayed Revenue Recognition
Pending authorizations can slow down claim approvals, causing delays in recognizing revenue for services provided.

Increased Administrative Burden
Manual paperwork and constant follow-ups add extra workload for staff, taking focus away from patient care.

Potential Revenue Loss
Denied or missed authorizations can result in unpaid claims, directly affecting provider income.
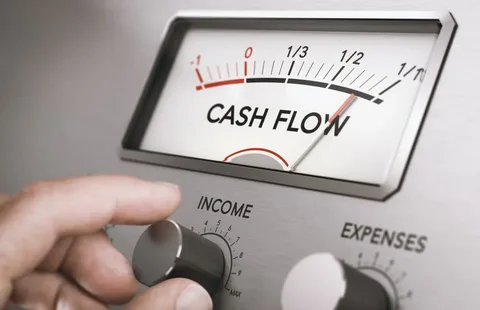
Effect on Cash Flow
Authorization delays create disruptions in cash flow, impacting the financial stability of healthcare practices.
Stay Ahead in Medical Billing
Specialties We deal with
Healthcare professionals can take advantage of our experience in a wide range of specialties by working
with SA Care Consultancy. We ensure that your billing and coding requirements are met accurately and promptly.
Scribe Align specializes in a range of medical billing and coding specialties, including:
Cardiology
Neurology
Oncology
Orthopedic
Dermatology
Urology
Family Medicine
Internal Medicine
Psychiatry
Radiology
Nephrology
Anesthesia
Why Choose Us for Pre & Retro Authorization Services

Rapid Revenue Recovery
25 Days

First-Pass Resolution
99 %

Denial & Rejection
5 % - 10%

Short Turnaround Time
24 Hours

Electronic Claim
95%

Electronic Payment
95%

Client Retention
100 %

Revenue Increase
30%
Trusted Softwares You’ll Recognize




















What Our Clients Says
Our clients trust us to deliver results — here’s what they have to say about their experience.
Their RCM support made patient payments smooth and predictable—we finally have consistent cash flow.
My clinic’s website started ranking locally in just two months, and appointments are flowing in.
They helped me turn my idea into a real launch with clear steps and supportive guidance.
Outsourcing admin tasks freed up our time, and new partnership leads started coming in.
Our website is fast, clean, and easy for patients to use—exactly what we needed.
Accurate coding eliminated billing errors and helped us avoid denials.
They got our providers credentialed quickly—claims started processing sooner than expected.
Their process system made our billing cycle clear and easy to manage.
– Jessica Turner
Eligibility checks now happen upfront—no surprises, no delays.
They helped chase payments effectively—AR days dropped noticeably.
– Priya Singh
Denied claims got resolved fast—revenue bounced back immediately.
– Emily Jackson
The help desk is responsive and scheduling errors are now rare.
– Michael Lee
Their authorization follow-ups saved us so many denied pre-authorizations.
Their reports are tailored to our needs—easy to understand and very useful.
Simplify Pre & Retro Authorizations
Avoid treatment delays and claim denials with our expert authorization services. We handle approvals quickly so your patients get care faster—and your revenue stays secure.
frequently asked question
Pre-authorization is the approval process required by insurance companies before certain medical services, treatments, or prescriptions are provided. It ensures medical necessity and coverage.
Prior authorization helps providers secure timely approvals, reduce claim denials, and ensure services are reimbursed by insurance without delays.
Most payers require patient medical records, physician notes, treatment plans, and insurance details to process a prior authorization.
Retro authorization is the process of obtaining approval from the insurance company after the service has already been provided, often required in emergencies or unavoidable circumstances.
Retro authorization is needed if pre-authorization was missed due to urgent care, system errors, or when services were provided before insurance details were available.
Our team promptly reviews denial reasons, submits appeals, and provides complete documentation to resolve and secure approval efficiently.